Gender disparities in high-risk pulmonary embolism: a nationwide analysis of management strategies and clinical outcomes | BMC Cardiovascular Disorders

Of a total of 1,105,295 patients with a primary diagnosis of acute PE, 45,140 (4.1%) were classified as having high-risk and were included in this analysis. The study population comprised 21,965 (48.6%) male and 23,275 (51.4%) female patients. Female patients were significantly older than male patients (mean age 65.2 vs. 63.4 years, p < 0.001). Regarding ethnicity, White patients constituted the majority in both groups, but with a higher proportion among males (66.5% vs. 62.1%), while Black patients were more prevalent among females than males (26.5% vs. 21.9%, p < 0.001).
In terms of record characteristics, female patients had a higher incidence of cardiac arrest (35.4% vs. 30.4%, p < 0.001) and acute cor pulmonale (24.2% vs. 21.7%, p < 0.001), while male patients more frequently presented with ventricular fibrillation (4.2% vs. 3.2%, p < 0.001) and ventricular tachycardia (8.3% vs. 6.2%, p < 0.001).
Regarding comorbidities, female patients had a higher prevalence of valvular heart disease (8.9% vs. 7.2%, p < 0.001), chronic lung disease (25.4% vs. 24.0%, p < 0.001), obesity (28.5% vs. 21.9%, p < 0.001), and anemia (44.4% vs. 38.2%, p < 0.001). Conversely, male patients more frequently had heart failure (37.1% vs. 33.5%, p < 0.001), atrial fibrillation/flutter (27.2% vs. 20.5%, p < 0.001), dyslipidemia (31.8% vs. 31.2%, p = 0.169), smoking history (35.8% vs. 25.9%, p < 0.001), and hematologic malignancy (14.2% vs. 11.5%, p < 0.001). A complete list of comorbidities and their prevalence is provided in Table 1.
In-hospital procedures and outcomes
Crude rates
Table 2 showed the analysis of in-hospital management and clinical outcomes of patients with high-risk PE stratified by gender. Regarding management strategies, female patients were significantly more likely to receive systemic thrombolysis compared to male patients (17.5% vs. 15.5%, p < 0.001). However, Male patients had numerically higher rates of catheter-directed thrombolysis (7.3% vs. 7.0%, p = 0.260) and catheter-directed embolectomy (7.5% vs. 7.2%, p = 0.130), but these differences were not statistically significant. Males were also more likely to undergo surgical embolectomy/thrombectomy (2.9% vs. 2.5%, p = 0.002) and receive IVC filter placement (15.2% vs. 14.3%, p = 0.008). Females had marginally higher rates of ultrasound-facilitated catheter-directed thrombolysis (1.5% vs. 1.4%, p = 0.363), but this difference was not statistically significant.
In terms of clinical outcomes, female patients experienced significantly higher rates of all-cause mortality (45.5% [26060] vs. 42.1% [20370], p < 0.001) and major adverse cardiovascular and cerebrovascular events (MACCE) (49.6% vs. 45.5%, p < 0.001). The incidence of major bleeding was similar between genders (13.8% for females vs. 13.6% for males, p = 0.033). When examining specific types of bleeding, intracranial hemorrhage (ICH) rates were identical (3.2% for both genders, p = 0.713), gastrointestinal bleeding was more common in male patients (8.2% vs. 7.5%, p = 0.004), retroperitoneal bleeding was significantly more frequent in females (2.5% vs. 1.3%, p < 0.001), and procedure-related bleeding was slightly more prevalent in female patients (1.0% vs. 0.9%, p < 0.001).
Male patients had a longer mean length of stay compared to female patients (9.8 days vs. 8.9 days, p < 0.001) and the mean total hospital charges were higher for male patients ($186,559.7 vs. $172,881.0, p < 0.001).
Figure 2 illustrates the disposition of patients with high-risk PE stratified by gender. Male patients were more likely to be discharged directly home compared to female patients (69.3% vs. 60.3%). Conversely, female patients had higher rates of discharge to intermediate care facilities (15.7% vs. 11.1%) and home health care services (18.2% vs. 13.1%). Male patients were slightly more likely to be discharged to short-term facilities (2.3% vs. 1.9%) and to leave against medical advice (1.2% vs. 0.7%). These gender-based differences in disposition were all statistically significant, with p-values less than 0.001.
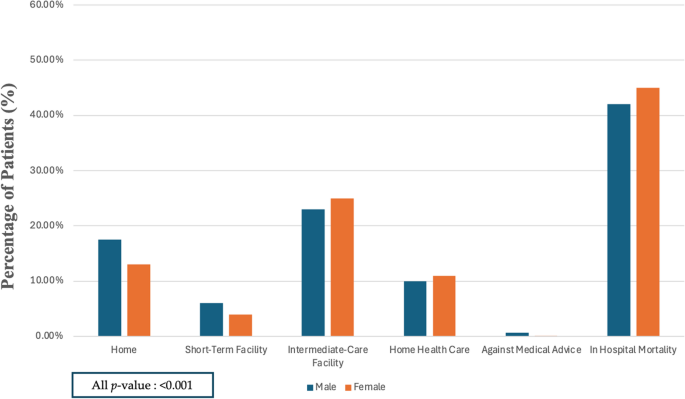
Disposition of patients with high-risk pulmonary embolism stratified by gender
Multivariable logistic analysis
The multivariate analysis showed several significant findings (Table 3). After adjusting for various factors, females were significantly more likely to receive systemic thrombolysis (aOR 1.17, 95% CI 1.11–1.23, p < 0.001) compared to males. However, they were less likely to undergo certain invasive procedures, including catheter-directed embolectomy (aOR 0.92, 95% CI 0.86–0.99, p = 0.034), surgical embolectomy/thrombectomy (aOR 0.83, 95% CI 0.73–0.93, p = 0.002), and IVC filter placement (aOR 0.86, 95% CI 0.82–0.91, p < 0.001). Interestingly, there were no statistically significant differences between genders in the use of catheter-directed thrombolysis (aOR 0.97, 95% CI 0.90–1.04, p = 0.406) or ultrasound-facilitated catheter-directed thrombolysis (aOR 1.08, 95% CI 0.92–1.27, p = 0.338).
In terms of clinical outcomes (Table 3; Fig. 3), female patients experienced significantly higher risk of MACCE (aOR 1.21, 95% CI 1.16–1.25, p < 0.001) and all-cause mortality (aOR 1.22, 95% CI 1.18–1.27, p < 0.001). Interestingly, there were no significant differences in the risk of major bleeding (aOR 0.99, 95% CI 0.93–1.05, p = 0.669) or intracranial hemorrhage (ICH) (aOR 0.97, 95% CI 0.87–1.08, p = 0.620) between genders after adjustment.
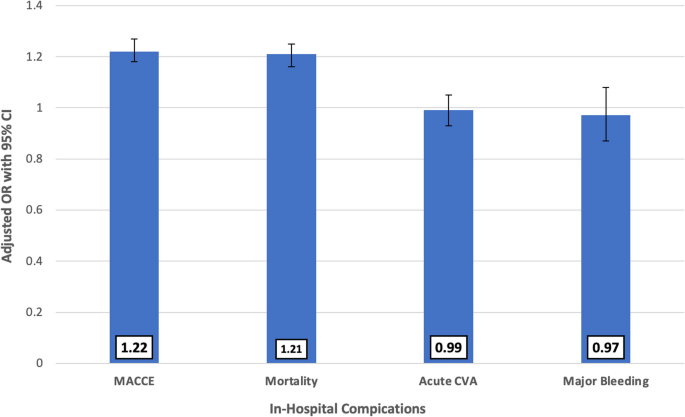
Gender-based multivariate analysis of In-hospital complications in patients with high-risk pulmonary embolism
link





